Why Medical Billing Audits in 2026 Are More Critical Than Ever
- Med Cloud MD
- Feb 3
- 8 min read
Updated: Feb 8

Medical billing audits in 2026 hit practices harder than ever. Payers recovered $3.3 billion through fraud investigations last year. Common triggers: duplicate claims, missing documentation, excessive modifier use, and billing patterns that don't match your specialty. RAC audits went from random samples to AI-driven targeting. Most practices get 30-100 chart requests with 14-30 days to respond. One skilled nursing facility owed back $243,000 after a cost report audit. Prevention beats panic: run internal audits quarterly, verify every claim before submission, and keep documentation for 7 years minimum.
Picture this: you're in the middle of a packed clinic day. Between patient visits, you notice an email from Medicare with "Audit Notice" in the subject line.
Your stomach drops. They're requesting 50 patient charts from the last two years. You have 21 days to respond. And you're not entirely sure your documentation will hold up under scrutiny.
This isn't some horror story from a blog. It's happening to practices everywhere right now. Small clinics, large groups, solo docs nobody's off limits anymore.
Medical billing audits in 2026 aren't like they used to be. Payers aren't just checking for fraud. They're using AI to spot patterns, flag outliers, and identify practices whose billing looks even slightly different from the norm. And when they find something, they're aggressive about getting money back.
Here's what you need to know to protect your practice before an audit letter shows up.

What Actually Happens During a Medical Billing Audit
An audit is when someone insurance company, Medicare contractor, or government agency reviews your claims and documentation to make sure you got paid the right amount for services you actually provided and documented correctly.
Who's doing the auditing:
Insurance companies review claims they've already paid, looking for reasons to take money back. They call it "post-payment review."
RAC auditors (Recovery Audit Contractors) work for Medicare. They get paid a percentage of whatever overpayments they find, so they're motivated to dig deep.
Medicare Advantage plans face RADV audits (Risk Adjustment Data Validation) where CMS verifies diagnosis codes. They estimate $22-43 billion in overpayments annually just in MA.
ZPIC and UPIC contractors investigate suspected fraud. These aren't routine audits they are serious investigations that can freeze your payments while they dig through everything.
Your own practice should be running internal audits to catch problems before outside auditors do.
Why Audits Hit Harder in 2026
AI Is Doing the Hunting
Payers stopped relying on random sampling. They're using software that compares your billing to thousands of other providers in real-time. Bill differently than your specialty's norm? You get flagged. Simple as that.
CMS announced they're expanding audit staff from 40 medical coders to 2,000 by September. That's not for decoration they are planning to audit every eligible Medicare Advantage contract annually.
Documentation Failures Are Everywhere
Know why most audits fail? Not fraud. Not intentional errors. Missing documentation.
A recent review found 40% of flagged claims had documentation problems. Notes were vague. Medical necessity wasn't clear. Time wasn't documented. Supporting records were missing.
AI can now scan your notes and flag documentation gaps automatically. If your chart doesn't clearly establish why the patient needed that specific service, the claim gets questioned.
They're Coming After Medicare Advantage Hard
CMS is finishing all backlogged RADV audits from 2018-2024, then moving to annual audits of every eligible plan. Even if you don't participate in MA plans directly, this signals how serious CMS has gotten about verification.
The Money Gets Serious Fast
It's not just "oops, we need that payment back." Penalties exist. Corrective action plans get mandated. Future audits increase. And in bad cases, providers can be excluded from Medicare entirely.
One skilled nursing facility got hit for $1.7 million in overstated costs across 7 locations averaging $243,000 per facility. Another home health agency in San Diego faced $5.9 million in projected overbilling from a Medicare audit.
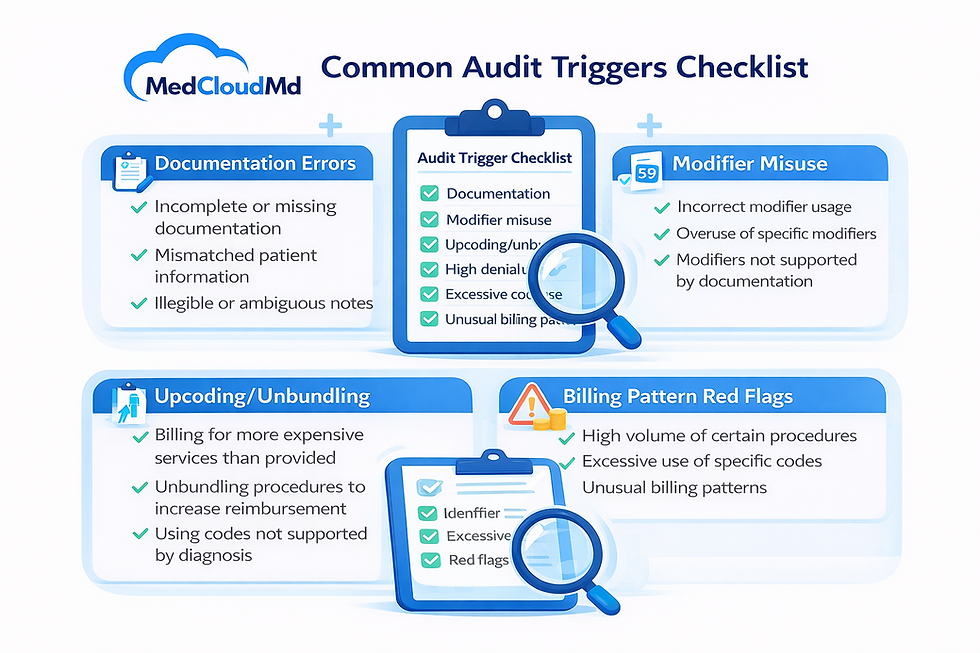
What Triggers an Audit (And How to Avoid It)
Duplicate Claims
Submitting the same claim twice whether by accident or system error is one of the fastest ways to trigger scrutiny. Payers flag duplicates instantly.
How it happens: Claim doesn't show as received in your system, so staff resubmits. Or your software glitches and sends it twice.
How to prevent it: Track every claim submission. Check claim status before resubmitting. Use software that prevents duplicate entries.
Missing Documentation
If your medical record doesn't fully support what you billed, auditors question everything.
What's missing:
Provider signature
Clear link between diagnosis and service
Time documentation for time-based codes
Medical necessity justification
Supporting test results or imaging
The fix: Create documentation checklists by service type. Make your EMR flag incomplete notes before they can be closed.
Billing for Medically Unnecessary Services
Payers deny claims when the service doesn't match the patient's clinical need.
Red flags:
Diagnostic tests that don't fit the presenting problem
Treatment frequency that exceeds clinical guidelines
Procedures billed without exam findings supporting them
Services that seem excessive for the diagnosis
The fix: Document why each service was necessary based on the patient's condition, exam findings, and clinical judgment.
Excessive Modifier Use
Modifiers explain unusual billing situations. But use them too often and it looks like you're gaming the system to bypass claim edits.
Problem modifiers:
25 (significant E/M on procedure day) used on every procedure
59 (distinct service) to unbundle codes that should be reported together
Modifier combinations that don't make clinical sense
The fix: Only use modifiers when truly warranted. Train staff on proper modifier application. Audit modifier usage quarterly.
Billing Patterns That Don't Match Your Specialty
AI compares your billing to national averages. If your numbers are way off, you get reviewed.
Patterns that trigger audits:
Billing highest-level E/M codes 90% of the time
Sudden spikes in claim volume or complexity
High use of specific high-paying procedures
Billing frequencies that exceed peer norms
What Happens If You Get Audited
Payment Takebacks Hurt Immediately
The most direct hit: payers demand refunds on claims they already paid. These recoupments can cover multiple years depending on audit type.
Real example: A family practice faced E/M coding audit. Documentation didn't support billed levels in 30% of sampled claims. Extrapolated over three years: $87,000 owed back.
Cash Flow Stops During the Audit
Some payers suspend new claim payments while the audit is ongoing. Your revenue stream freezes while you're scrambling to gather documentation and respond.
Penalties Can Add Up Fast
Beyond repayment, Medicare can impose penalties if they determine you showed "reckless disregard" for billing rules even without proving fraud.
Modifier errors? Some violations carry $10,000 fines per occurrence. Use the wrong modifier 20 times and you're looking at $200,000 in penalties.
Future Scrutiny Increases
Fail an audit and you're marked. Future claims get reviewed more carefully. You might face more frequent audits. Your practice is on a watch list.
Worst Case: Program Exclusion
In extreme situations, providers can be excluded from Medicare and Medicaid programs. For most practices, that effectively ends your ability to operate.
How to Actually Prepare for Audits
Document Like Someone's Watching (Because They Are)
Every note should answer: why did this patient need this specific service today?
What auditors look for:
Chief complaint clearly stated
History of present illness with specifics
Relevant exam findings documented
Clinical reasoning explaining service choices
Treatment plan tied to findings
Not acceptable: "Patient doing well. Continue current plan." That won't defend anything.
Better: "Type 2 diabetes with HbA1c 8.2% despite metformin 1000mg BID. Added glipizide 5mg daily. Recheck labs in 6 weeks. Discussed diet modifications and referred to diabetes educator."
Run Internal Audits Before Payers Do
Don't wait for an audit notice to find out your documentation has problems.
Internal audit schedule:
Random chart reviews monthly (10-15 charts)
Focused audits on high-risk services quarterly
Annual comprehensive compliance review
Pre-submission claim scrubbing for high-dollar claims
Keep Everything for 7 Years Minimum
Some audits look back 3-6 years. Fraud investigations can go back further. You need documentation available immediately when requested.
What to keep:
Complete medical records
All claim documentation
Authorization records
Payer communications
Denial and appeal records
Payment records and EOBs
Train Staff on Current Rules
Most errors happen because staff don't know rules have changed.
Training topics:
Annual CPT and ICD-10 updates
Modifier usage and requirements
Payer-specific policies
Documentation standards
Compliance procedures
Verify Claims Before They Go Out
Catching errors before submission prevents denials and audit triggers.
Pre-submission checks:
Code accuracy against documentation
Required modifiers present and correct
Diagnosis supports service medical necessity
Time documented for time-based codes
Authorization active and covers service
How MedCloudMD Keeps Practices Audit-Ready
At MedCloudMD, we built our billing around compliance because we know audit risk is real and expensive.
Every Claim Gets Reviewed Before Submission
Our certified coders check documentation, verify code accuracy, confirm medical necessity, and validate modifiers before claims leave your practice. We catch the errors that trigger audits.
We Track Denial Patterns and Fix Root Causes
Repeated denials signal systemic problems that will eventually trigger audits. We analyze why claims get denied, identify patterns, and implement fixes so the same errors stop happening.
State-Specific Compliance Expertise
Medicaid rules vary by state. Commercial payer policies differ. We track requirements across all your payers and apply the right rules to each claim automatically.
Internal Audit Support
We conduct regular compliance reviews of your billing, identifying potential audit triggers before outside auditors find them. You get detailed reports showing exactly where risk exists and how to fix it.
Rapid Audit Response
If you receive an audit notice, we organize requested documentation fast, review audit samples for accuracy, identify issues, and help you respond effectively to minimize financial impact.
Check our revenue cycle services →
Questions Providers Keep Asking
What triggers a medical billing audit?
Common triggers include duplicate claims, missing documentation, excessive modifier use, billing patterns that deviate from specialty norms, high denial rates, and random selection. AI now flags unusual patterns automatically.
How long do I have to respond to an audit?
Typically 14-30 days depending on the payer and audit type. RAC audits usually give 30 days. Commercial payers vary. Respond quickly extensions are rare and missing deadlines weakens your position.
Can they audit claims from years ago?
Yes. Most audits look back 3-6 years. Fraud investigations can go back further. Medicare can review claims up to 7 years in some cases. Always keep documentation for at least 7 years.
Should I run internal audits even if I haven't been audited?
Absolutely. Internal audits find problems before external auditors do, identify revenue you're missing, reduce denials, and demonstrate good-faith compliance if you are audited externally.
What happens if I can't produce the requested documentation?
If you can't provide documentation supporting a billed service, that claim gets denied and you repay the payer. Multiply that across all sampled claims and the financial impact gets severe fast.
Can I appeal audit findings?
Yes, but success varies. You need strong supporting documentation and clear clinical justification. Many audit denials are upheld because documentation genuinely doesn't support what was billed.
How much does failing an audit actually cost?
Beyond repaying claims, you face potential penalties, legal costs, increased audit frequency, and administrative time. Real examples range from $30,000 to millions depending on scope and violations found.
Don't Wait for an Audit Notice to Fix Your Billing
Medical billing audits in 2026 aren't theoretical. They're happening right now to practices that thought they were safe.
The practices that survive audits without major financial hits aren't lucky. They're prepared. They document thoroughly. They code accurately. They audit themselves before payers do. And they work with billing partners who prioritize compliance over just pushing claims through.




Comments