Rheumatology Prior Authorization Rules: Best Practices to Get Faster Approvals in 2026
- Med Cloud MD
- 16 hours ago
- 8 min read

If you have ever waited three weeks for a biologic prior authorization only to have it denied for missing documentation, you know how frustrating rheumatology prior authorization rules can be. Between payer-specific criteria that change quarterly, step therapy requirements that aren't always clear, and biologics that cost $4,000 per dose, getting PAs approved quickly isn't just about avoiding headaches it's about keeping your practice financially healthy and your patients on the treatments they need.
Understanding Prior Authorization in Rheumatology
Prior authorization is the insurance company saying 'prove this treatment is necessary before we'll pay.' It's cost control for high-dollar services, which includes most rheumatology care biologics, infusions, certain imaging and procedures.
You submit clinical documentation showing why the patient needs this treatment, the payer reviews it against their policy, and they approve, deny, or request more information. The process takes 48 hours to several weeks depending on the payer and how complete your submission was.
Why Prior Authorization Matters More Than Ever in 2026
Payers are getting tougher, using AI to flag requests that don't match their criteria perfectly. They're requiring more upfront documentation and enforcing step therapy more strictly.
Biologics keep getting more expensive. When Remicade costs $3,800 per infusion and Stelara runs $12,000 per dose, payers want proof cheaper options failed first, dosing is appropriate, and the diagnosis truly requires this medication.
Practice guidelines change frequently. What worked for PA last year might fail this year because payers updated policies or CMS issued new coverage rules. Miss these changes and denials seem arbitrary but are actually policy updates you didn't catch.
Rheumatology Prior Authorization Rules by Payer Type
Medicare Prior Authorization Requirements
Medicare traditionally didn't require much PA, but that's changing. They've rolled out programs for certain high-cost drugs and are expanding coverage each year.
The biggest pitfall? Assuming they don't require it. Some biologics fall under Part B and may need PA depending on your MAC. Others are Part D through prescription plans and definitely need PA. Documentation must show medical necessity clearly diagnosis codes matching approved indications, previous treatments tried, disease activity evidence, and clinical rationale for this medication over alternatives.
Medicaid Prior Auth Rules
Medicaid is tricky because every state runs differently. Texas Medicaid has completely different PA rules than New York. What works in one state won't necessarily work in another.
Most state programs maintain preferred drug lists. If your medication isn't on the list, you're proving the patient tried and failed preferred options first that's step therapy. PA windows vary too some states want 10 business days advance notice, others accept shorter timeframes.
Commercial Payers and Biologics
Commercial insurance is where PA gets really complicated. Every payer has their own policies, step therapy protocols, and documentation requirements. What Blue Cross accepts might completely differ from United Healthcare's needs.
Biologics almost always trigger PA for commercial plans. They want proof conventional DMARDs failed, the patient meets disease severity criteria, and there's no contraindication. Benefit verification is critical even within one payer like Anthem, different plans cover biologics differently. Verify the specific plan's requirements.

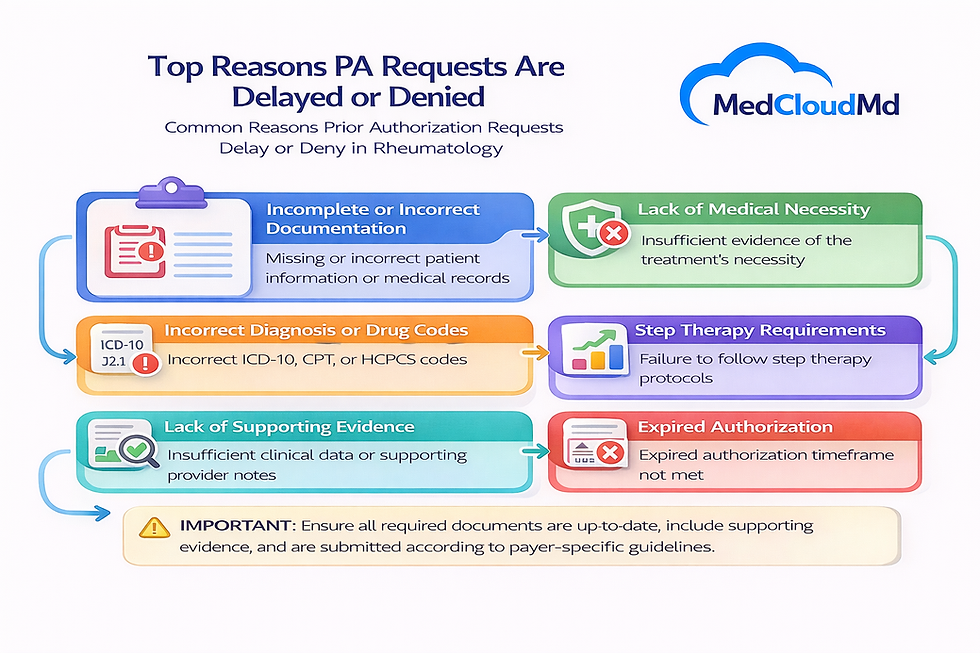
Why Biologics and Infusion Prior Auth Requests Fail
The number one reason? Incomplete documentation. Missing lab work showing disease activity, forgotten notes about failed methotrexate trials, or undocumented reasons why the patient can't tolerate preferred medications.
Step therapy is another common failure. The payer requires two DMARD trials before approving biologics, but your documentation shows only one. Or you documented failures but didn't include dosages and duration, so the payer can't verify trials were adequate.
Payer-specific criteria trip people up constantly. Cigna requires three months of DMARD therapy, you documented six weeks. Aetna covers Orencia only after Humira failure, you went straight to Orencia. Without documenting medical rationale for deviating from their sequence, they deny it.
Response time delays create their own problems. If a payer takes 15 business days to review and comes back asking for additional information, and then takes another 10 days after you send it, you're now a month into this process. Meanwhile the patient needs the medication.
Retroactive PA is basically a fantasy. Some practices think they can administer the medication and get authorization later if the patient urgently needs it. Maybe one in ten payers will consider retroactive authorization, and even then, success is not guaranteed. Plan for prospective authorization always.
Getting Prior Authorization Approved Faster
Start With Accurate Information Upfront
Before you submit anything, verify the patient's current coverage. Not what they had last quarter what they have right now. Check if the specific medication needs PA for this specific plan. Get the correct forms or portal process for this payer.
Capture plan-specific requirements while you're at it. Does this payer require a specific specialty pharmacy? Do they need the prescription sent to a certain location? Is there a preferred provider network for infusions? Getting these details up front prevents delays later.
Know What Each Payer Actually Wants
Don't guess at requirements. Look up the actual medical policy. Most payers publish their PA criteria online you just need to find it and read it. What diagnoses do they approve this medication for? What's their step therapy protocol? What lab values or assessments do they expect to see?
Track policy updates. Set calendar reminders to review major payer policies quarterly. Subscribe to payer newsletters if they offer them. Or work with someone who tracks this professionally, because keeping up with 15+ payers' changing rules is basically a full-time job.
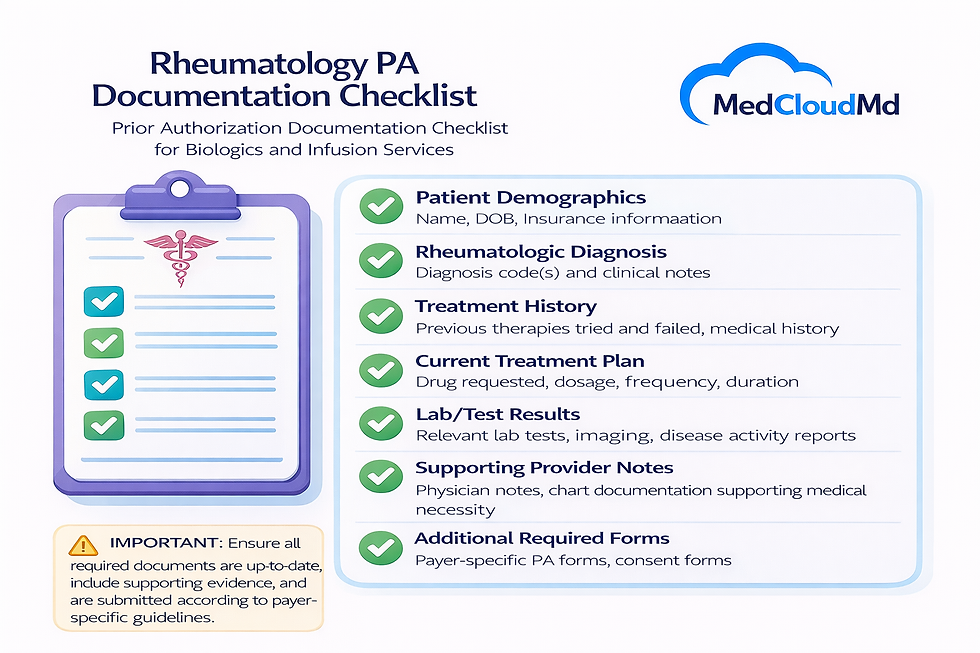
Prepare Complete Clinical Documentation
Include everything the first time. Labs showing inflammatory markers, imaging demonstrating joint damage or progression, clinical notes detailing functional limitations, documented trials of previous medications with specific dates, dosages, and reasons for discontinuation.
For step therapy documentation, be specific. Don't just say 'patient failed methotrexate.' Say 'patient tried methotrexate 20mg weekly for 16 weeks, developed elevated liver enzymes with AST 89 and ALT 112, discontinued due to hepatotoxicity per lab results dated [date].' The more specific you are, the harder it is for them to deny.
Use Templates and Checklists
Create standardized PA submission templates for the biologics you commonly prescribe. Pre-fill the required fields, create checklists of needed documentation, build in reminders for payer-specific requirements. This prevents omissions that cause denials.
Checklists sound basic, but they work. Having a one-page checklist that says 'For Humira PA you need: diagnosis, CRP/ESR within 30 days, two previous DMARD trials with dates, current joint count, functional assessment' prevents you from submitting incomplete requests.
Track Everything and Follow Up
Don't just submit the PA and hope for the best. Track submission dates, expected response dates, follow-up dates if you haven't heard back. Use a spreadsheet, a dashboard in your practice management system, or dedicated PA tracking software.
Follow up proactively. If the payer says they need 10 business days and you're on day 9 without an answer, call them. If they say they're missing documentation, get it to them immediately, don't wait another week. Every day of delay is another day your patient doesn't get the treatment they need.
Train Your Staff
Everyone who touches the PA process needs training front desk staff who verify insurance, clinical staff who gather documentation, billing staff who submit requests. Create standard operating procedures, hold regular training sessions, and update everyone when payer policies change. A well-trained team gets PAs approved faster.
How PA Delays Impact Your Practice
When prior authorization drags out or gets denied, you're not just inconveniencing the patient you're creating revenue cycle problems. If you administer a biologic without approved PA, that claim is getting denied and you're stuck trying to appeal or write it off.
Patient access suffers. Someone in an RA flare who needs Orencia next week but PA takes three weeks is in pain longer than necessary. That affects patient satisfaction, treatment outcomes, and whether they stay with your practice or find another provider.
Days in AR climb when services get delayed. That expensive infusion you would have billed this month gets pushed to next month, and if the PA ultimately gets denied, you're spending staff time on appeals instead of collecting on clean claims. The financial ripple effects are real.
Real-World Prior Authorization Scenarios
Scenario 1: Biologic Denied for Incomplete Step Therapy Documentation
What happened: Practice requested PA for Enbrel. United Healthcare denied it, stating insufficient evidence of conventional DMARD failure.
The problem: The provider's note mentioned previous methotrexate use but didn't include specific dates, dosage, duration, or documented reason for discontinuation. Payer couldn't verify adequate trial.
Resolution: Practice gathered detailed records showing methotrexate 20mg weekly for 14 weeks with persistent disease activity (CRP 24, joint count 8) and gastrointestinal intolerance requiring discontinuation. Resubmitted with complete documentation. PA approved within 5 days.
Scenario 2: Infusion Authorization Delayed by Missing Labs
What happened: Submitted PA for Remicade infusion. Aetna requested additional information, delaying approval by two weeks.
What was missing: Current CRP and ESR values. Payer policy required labs within 60 days of PA submission, but practice sent labs from 4 months prior.
The fix: Ordered fresh labs, submitted within 48 hours, PA approved. Practice implemented checklist requiring current labs before any biologic PA submission to prevent recurrence.
How MedCloudMD Supports Prior Authorization Workflows
We work with rheumatology practices specifically because we understand that PA isn't just paperwork it's a critical part of your revenue cycle that directly impacts patient care and cash flow.
Our team tracks payer-specific PA requirements, maintains documentation templates for common biologics, verifies coverage before services, submits complete requests the first time, and follows up systematically until approval. Learn more about our rheumatology billing services.
When denials happen, we don't just appeal we figure out why it was denied and fix the root cause so it doesn't keep happening. The goal is faster approvals, fewer denials, and less administrative burden on your clinical staff.
Questions About Rheumatology Prior Authorization
What is prior authorization in rheumatology?
Prior authorization is approval from the insurance company before providing certain services or medications. In rheumatology, it's most commonly required for biologics, infusions, high-cost imaging, and certain procedures. You submit clinical documentation showing medical necessity, and the payer reviews it against their coverage criteria.
Why do biologic PA requests get denied?
Common reasons include incomplete step therapy documentation, missing clinical evidence of disease activity, outdated lab results, failure to show previous treatment trials with adequate dosing and duration, not meeting payer-specific severity criteria, or requesting non-preferred medications without justification.
How far in advance should I request prior authorization?
Start PA requests at least 2-3 weeks before the planned service date. Some payers respond in 48-72 hours, others take 10-15 business days. Factor in time for potential requests for additional information. For urgent situations, call the payer to request expedited review, though approval isn't guaranteed.
What documentation do payers require for infusion approval?
Typical requirements include diagnosis with ICD-10 codes, current disease activity markers (CRP, ESR, joint counts), history of conventional treatment trials with dates and outcomes, clinical notes explaining why this infusion is appropriate, recent labs showing the patient can safely receive the medication, and documentation that the patient meets payer-specific criteria for biologics.
Can prior authorization be appealed if denied?
Yes. Most payers have a formal appeals process with multiple levels. Submit additional clinical documentation supporting medical necessity, explain why the denial criteria don't apply or were misinterpreted, and provide any new evidence. Peer-to-peer reviews with the payer's medical director can also be requested and often improve approval chances.
Does prior authorization guarantee payment?
Not always. PA confirms the service is medically necessary and covered under the plan, but payment still depends on submitting a clean claim with correct coding, the patient having active coverage on service date, and meeting any other claim requirements. PA significantly improves payment likelihood but isn't an absolute guarantee.
Making Prior Authorization Work for Your Practice
Prior authorization doesn't have to be a constant source of frustration. With clear processes, complete documentation, payer-specific knowledge, and systematic tracking, you can get biologics and infusions approved faster and reduce denials significantly.




Comments